Index
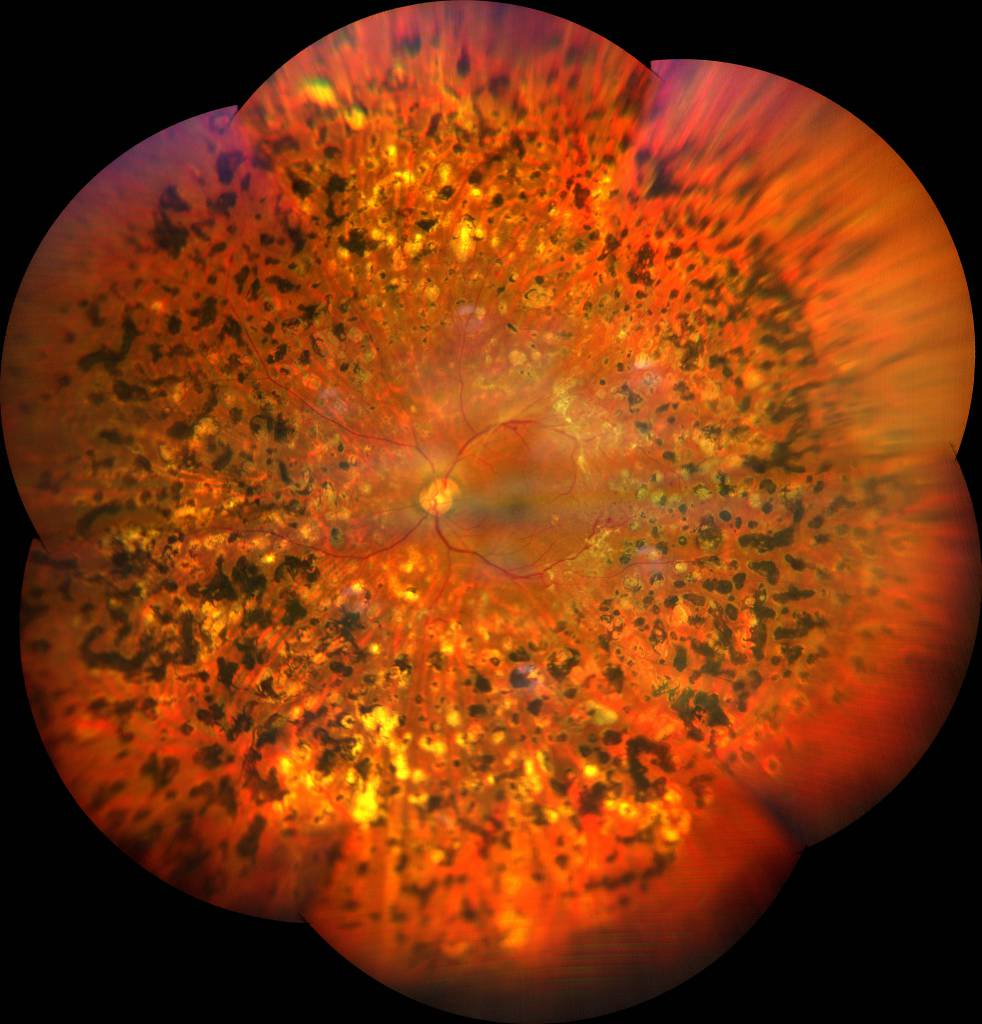
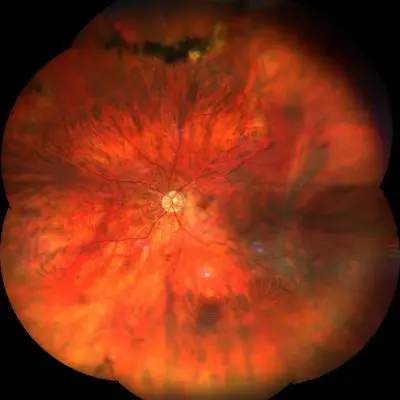
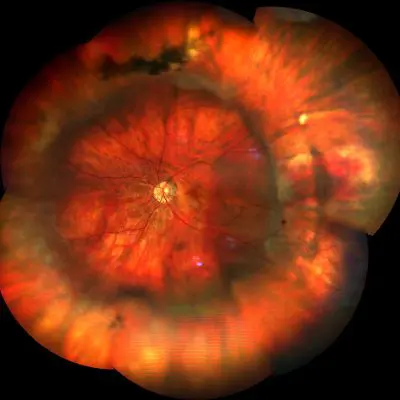
Proliferative diabetic retinopathy it is the most severe form of diabetic retinopathy and can severely and irreversibly impair vision.
Proliferative diabetic retinopathy (PDR) it is classified as early, high risk and severe. High risk is defined by moderate to severe neovascularization of the optic disc (> 1/3 -1/2 of the optic disc area), any neovascularization of the optic nerve if vitreous or pre-retinal hemorrhages are present, or a moderate to severe neovascularization anywhere on the retina (at least half of the optic disc area) if vitreous or pre-retinal hemorrhages are present.
Pathological neovascularization is caused by a state of hypoxia, i.e. poor oxygenation, induced by the presence of one or more ischemic areas in the retina. In such circumstances, the eye "responds" by promoting the growth of new blood vessels defined as "immature", which have a particularly fragile and altered structure.
The pathological new vessels do not efficiently oxygenate the retinal tissue on the contrary they damage it. In fact, they can give rise to small hemorrhages or to accumulation of plasma in the retina, causing the formation of a pseudo-fibrotic tissue. The coexistence of pseudo-fibrotic tissue and pathological new vessels can lead to vitreo-retinal proliferation and the formation of fibrovascular membranes.
These pseudo-cicatricial membranes that contract over time, deforming the retinal profile and causing distorted vision and decreased vision. If the fibrovascular membranes appear in the most central part of the retina, they can give rise to the appearance of dark areas (scotomas) in the visual field or even to the loss of central vision.
Neovascularization
Neovascularization is associated with pathological changes:
- Intraluminary cell proliferation, as well as changes in platelet function, erythrocyte aggregation, elevated plasma concentrations of fibrinogen resulting in vascular occlusion and ruptures. This causes small flame-shaped and spot-like hemorrhages near the occlusion and intraretinal infarcts (cottony exudates) distant from the occlusion.
- The proliferation of endothelial cells of the retinal veins resulting in a change in venous caliber
- Greater ischemia results in vasoproliferation with the formation of new vessels
The new vessels are categorized based on their presence, location, severity, and associated bleeding activity.
The proliferation of new vessels can also occur on the surface of the iris (rubeosis) and in the anterior chamber, blocking the outflow of aqueous humor and leading to acute glaucoma, a severe form of glaucoma that is difficult to control.
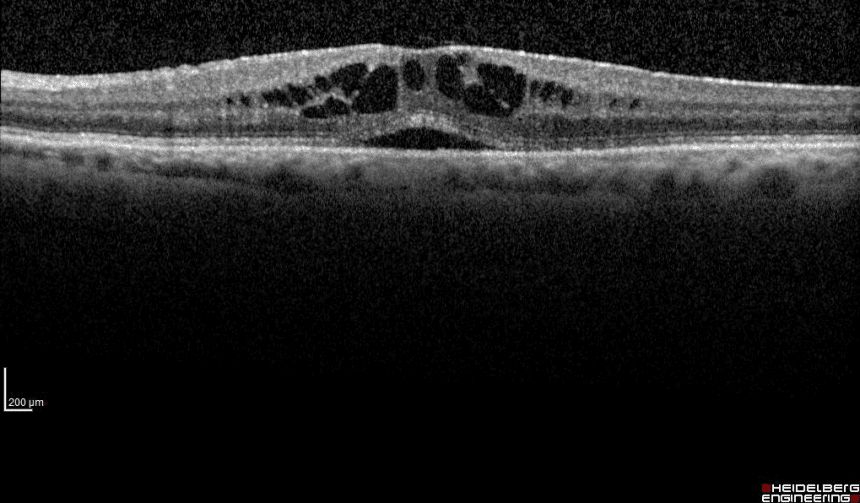
Fibrovascular membranes can evolve causing a loss of vision. When this occurs, they generate a contraction that causes traction on the retina to cause a detachment of the tractive retina. Sometimes the fibrovascular membrane thickens and wrinkles at the level of the macula, giving rise to a macular pucker. This complication, if not treated, can lead to a marked alteration of vision and sometimes evolve into a macular hole in need of emergency surgery.
Diagnosis
Proliferative diabetic retinopathy it is the most severe form of diabetic retinopathy and is capable of severely and irreversibly impairing vision. The main symptoms of this pathology are: blurring of central vision, difficulty in color perception and sometimes a reduction in night vision. The treatments available, although effective, do not always manage to safeguard the sight and are not always definitive. Therefore, the most effective weapon against this dangerous eye disease remains prevention.
It is obtained mainly through the strict control of blood glucose, and early diagnosis, which is implemented thanks to the careful and regular monitoring of the retina through tests such as: Optical Coherence Tomography (OCT) high resolution to examine every single retinal layer; Fluorescence Angiography with Fluorescein (FAG) e Indocyanine Green Angiography (ICGA) which are minimally invasive tests that use two contrast media, particularly useful for the identification of retinal new vessels.
These tests make it possible to diagnose diabetic retinopathy and, if necessary, to intervene promptly with the most appropriate treatment before serious damage to vision occurs. As an alternative to the above diagnostic means, theAngio-OCT, a non-invasive instrumental method that allows to acquire morphological data both of the retinal structure and of the microvascular complex of the retina and of the choriocapillary that facilitate the monitoring of patients.
Diabetic patients should start following a prevention protocol associated with regular retinal monitoring within the first year of diabetes diagnosis. Pregnant diabetic women must undergo particularly careful checks as early as the first trimester, as diabetic retinopathy can progress very rapidly during gestation.
Treatment
Most studies divided the surgical indication for PDR patients into the following groups:
- Vitreous hemorrhage
- Tractional rhegmatogenous retinal detachment
- Severe and progressive proliferative retinopathy
To avoid serious complications, such as a retinal detachment or macular pucker, which can cause total and irreversible loss of vision, a surgery called pars plana vitrectomy is required. This surgery aims to surgically remove the fibrovascular membranes, restoring vision and eliminating the danger of these serious complications.
In association with this type of intervention, an endolaser treatment is usually carried out during the same on the ischemic retinal areas, so that they do not give rise to new fibrovascular membranes, which could induce a relapse of the pathological process.
Pathology and treatment on video
Do you need more information?
Do not hesitate to contact me for any doubt or clarification. I will evaluate your problem and it will be my concern and that of my staff to answer you as quickly as possible.